WHAT IS DIABETES?
Diabetes is a problem with your body that causes blood glucose (sugar) levels to rise higher than normal. This is also called hyperglycemia.
When you eat your body breaks food down into glucose and sends it into the blood. Insulin then helps move the glucose from the blood into your cells. When glucose enters your cells, it is either used as fuel for energy right away or stored for later use. In a person with diabetes, there is a problem with insulin. But, not everyone with diabetes has the same problem.
There are different types of diabetes – type 1, type 2, and a condition called gestational diabetes, which happens during pregnancy. If you have diabetes, your body either doesn’t make enough insulin, it can’t use the insulin it does make very well, or both.
WHAT IS TYPE 1 DIABETES?
In type 1 diabetes, your immune system mistakenly destroys the cells in your pancreas that make insulin. Your body treats these cells as invaders and destroys them. This can happen over a few weeks, months, or years.
When enough beta cells are destroyed, your pancreas stops making insulin, or makes too little insulin. Because the pancreas does not make insulin, insulin needs to be replaced. Insulin does not come in a pill. People with type 1 diabetes take insulin by injection with a syringe, an insulin pen, or an insulin pump. Without insulin, your blood glucose rises and is higher than normal, which is called hyperglycemia.
Type 1 diabetes affects about 5% of people in the United States with diabetes. In the past type 1 diabetes was called juvenile diabetes or insulin-dependent diabetes. It’s usually first diagnosed in young people but it can occur at any age. Type 1 diabetes is much less common than type 2 diabetes.
HOW IS TYPE 1 DIFFERENT FROM TYPE 2?
In type 2 diabetes, your body does not use insulin properly. This is called insulin resistance. At first, the beta-cells make extra insulin to make up for it. But, over time your pancreas isn’t able to keep up and can’t make enough insulin to keep your blood glucose levels normal. Type 2 diabetes can be treated with oral medications, and/or insulin. Type 1 diabetes is always treated with insulin.
WHAT CAUSES TYPE 1 DIABETES?
Scientists aren’t sure what causes type 1 diabetes. It is not contagious and it is not caused by eating sugar. Research is under way to find the exact causes of type 1 diabetes and how it might be prevented.
WHAT IS DIABETES?
Diabetes is a problem with your body that causes blood glucose (sugar) levels to rise higher than normal. This is also called hyperglycemia.
When you eat your body breaks food down into glucose and sends it into the blood. Insulin then helps move the glucose from the blood into your cells. When glucose enters your cells, it is either used as fuel for energy right away or stored for later use. In a person with diabetes, there is a problem with insulin. But, not all people with diabetes have the same problem.
The types of diabetes are type 1, type 2, and a condition called gestational diabetes, which happens when pregnant. If you have diabetes, your body either doesn’t make enough insulin, it can’t use the insulin it does make very well, or both.
WHAT IS TYPE 2 DIABETES?
In type 2 diabetes, your body does not use insulin properly. This is called insulin resistance. At first, the pancreas makes extra insulin to make up for it. Over time your pancreas isn’t able to keep up and can’t make enough insulin to keep your blood glucose levels normal. Type 2 is treated it with lifestyle changes, oral medications (pills), and insulin.
Some people with type 2 can control their blood glucose with healthy eating and being active. But, your doctor may need to also prescribe oral medications or insulin to help you meet your target blood glucose levels. Type 2 usually gets worse over time – even if you don’t need medications at first, you may need to later on.
HOW IS TYPE 2 DIFFERENT FROM TYPE 1?
In type 1, your body treats the cells that make insulin as invaders and destroys them. This can happen over a few weeks, months, or years. When enough of the cells are gone, your pancreas stops making insulin, or makes too little insulin.
Without insulin, your blood glucose rises higher than normal, so the insulin needs to be replaced.
WHAT CAUSES TYPE 2 DIABETES?
Scientists do not know the exact cause of type 2 diabetes. However, development of type 2 diabetes has been associated with several risk factors. These risk factors include: Factors Affecting Blood Glucose
Before you had diabetes, no matter what you ate or how active you were, your blood glucose levels stayed within a normal range. But with diabetes, your blood glucose level can rise higher and some diabetes medications can make them go lower than normal. Many factors can change your blood glucose levels. Learning about these can help control your blood glucose levels.
You can use your blood glucose (sugar) levels to make decisions about food and activity. These decisions can help you delay or prevent diabetes complications such as heart attack, kidney disease, blindness, and amputation.
WHAT CAN MAKE MY BLOOD GLUCOSE RISE?
- Not being active
- Dehydration
- Too much food, like a meal or snack with more carbohydrates than usual
- Not enough insulin or oral diabetes medications
- Side effects from other medications, such as steroids, anti-psychotic medications
- Stress, which can produce hormones that raise blood glucose levels
- Menstrual periods, which cause changes in hormone levels
- Illness – your body releases hormones to fight the illness, and those hormones raise blood glucose levels
- Short- or long-term pain, like pain from a sunburn – your body releases hormones that raise blood glucose levels
WHAT CAN MAKE MY BLOOD GLUCOSE FALL?
- Side effects from other medications
- Alcohol, especially on an empty stomach
- Too much insulin or oral diabetes medications
- Not enough food, like a meal or snack with fewer carbohydrates than usual, missing a meal or snack
- More physical activity or exercise than usual – physical activity makes your body more sensitive to insulin and can lower blood glucose.
HOW CAN I TRACK MY BLOOD GLUCOSE?
There are two ways to keep track of your blood glucose levels:
- using a blood glucose meter to measure your blood glucose level at that moment
- getting an A1C at least twice a year to find out your average blood glucose for the past 2 to 3 months
TYPE 1 DIABETES
Symptoms of type 1 diabetes are serious and usually happen quickly. Most people with type 1 diabetes will feel very sick because of high blood glucose levels.
Common Signs and Symptoms of Type 1 Diabetes:
- Feeling very thirsty (due to dehydration)
- Urinating a lot (as the body tries to flush out excess glucose in the blood)
- Feeling hungry all the time (because the cells of the body are starved for energy)
- Feeling tired (because the glucose is not entering your cells and being converted to energy)
- Blurred vision (because of a buildup of fluid in the lens of your eyes caused by high blood glucose levels)
- Losing weight suddenly without trying, even with increased appetite (because the body is not able to use the food you eat)
- Nausea and vomiting (as a result of the buildup of ketones in the blood) Some people with type 1 diabetes may experience diabetic ketoacidosis.
TYPE 2 DIABETES
Type 2 diabetes does not appear suddenly. Instead, you may have no noticeable symptoms or only mild symptoms for years before it is diagnosed.
Common Signs and Symptoms of Type 2 Diabetes:
- Frequent infections or slow healing cuts and sores
- Tingling, pain, or numbness in the hands or feet
- Urinating a lot (as the body tries to flush out excess glucose in the blood)
- Feeling very thirsty (due to dehydration)
- Feeling hungry all the time (because the cells of the body are starved for energy)
- Feeling tired (because the glucose is not entering your cells and being converted to energy)
- Blurred vision (because of a buildup of fluid in the lens of your eyes caused by high blood glucose levels)
WHAT CAN I DO?
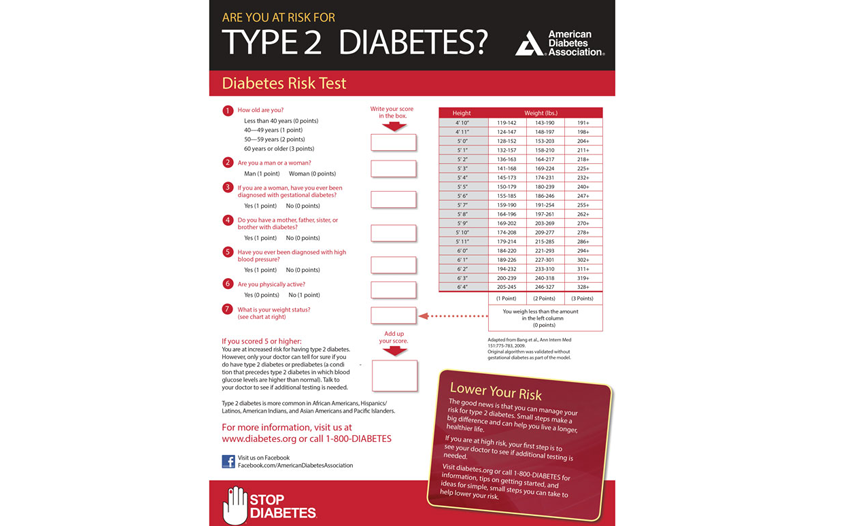
Early detection and treatment of diabetes can decrease the risk of developing the complications of diabetes. Talk to your doctor about being tested if you feel like you may have diabetes. Take our Risk Test (www.diabetes.org/risktest) to find out if you are at increased risk for having type 2 diabetes.
The first way to treat type 2 diabetes is often meal planning, weight loss, and exercise. Often these steps are not enough to bring blood glucose levels down to a healthy range. The next step is taking medication that lowers blood glucose levels.
Your doctor will decide which medication is right for you.
This depends on:
-
your lifestyle
-
how you respond to the medicine
-
physical condition
-
insurance coverage
ORAL MEDICATIONS
There are different types, or classes, of drugs that work in different ways to lower blood glucose.
1. Sulfonylureas chlorpropamide, (Diabinese), glipizide (Glucotrol and Glucotrol XL), glyburide (Micronase, Glynase, and
Diabeta), glimepiride (Amaryl)
Sulfonylureas stimulate the beta cells of the pancreas to release more insulin.
2. Biguanides metformin (Glucophage)
Biguanides lower blood glucose levels primarily by decreasing the amount of glucose produced by the liver. They also help to lower
blood glucose levels by making muscle tissue more sensitive to insulin so glucose can be absorbed.
3. Meglitinides repaglinide (Prandin), nateglinide (Starlix)
Meglitinides are drugs that also stimulate the beta cells to release insulin.
4. Thiazolidinediones rosiglitazone (Avandia), pioglitazone (ACTOS)
Thiazolidinediones drugs help insulin work better in the muscle and fat and also reduce glucose production in the liver.
5. DPP-4 Inhibitors sitagliptin (Januvia), saxagliptin (Onglyza), linagliptin (Tradjenta), alogliptin (Nesina)
DPP-4 Inhibitors work by preventing the breakdown of a naturally occurring compound in the body, GLP-1. GLP-1 reduces blood glucose
levels in the body, but is broken down very quickly so it does not work well when injected as a drug itself. By interfering in the
process that breaks down GLP-1, DPP-4 inhibitors allow it to remain active in the body longer, lowering blood glucose levels only when
they are high.
6. SGLT2 Inhibitors canagliflozin (Invokana), dapagliflozin (Farxiga), empagliflozin (Jardiance) Glucose in the blood passes through the kidneys. Sodium-glucose transporter 2 (SGLT2) works naturally in the kidney to reabsorb glucose, and SGLT2 inhibitors block this action, causing excess glucose to be eliminated in the urine.
7. Alpha-Glucosidase Inhibitors acarbose (Precose), meglitol (Glyset)
Alpha glucosidase inhibitors help the body to lower blood glucose levels by blocking the breakdown of starches, such as bread, potatoes,
and pasta in the intestine. They also slow the breakdown of some sugars, such as table sugar. Their action slows the rise in blood
glucose levels after a meal.
8. Bile Acid Sequestrants (BAS) colesevelam (Welchol)
The BAS colesevelam is a cholesterol-lowering medication that also reduces blood glucose levels in patients with diabetes.
9. Oral Combination Therapy
Because the drugs listed above act in different ways to lower blood glucose levels, they may be used together. For example, a biguanide
and a sulfonylurea may be used together. Many combinations are prescribed together as a single pill for convenience.
INSULIN
There are different types of insulin that vary in how quickly they lower blood glucose levels. Some work very quickly and are taken with meals. Others are long-acting and are used just once or twice a day.
1. Rapid Acting insulin glulisine (Apidra), insulin lispro (Humalog), insulin aspart (NovoLog) Onset:
about 15 minutes
Peak: about 1or 2 hours after injection
Duration: last between 2-4 hours
2. Regular or Short-Acting regular (Humulin R and Novolin R) Onset: about 30 minutes
Peak: about 2 to 3 hours after injection
Duration: last between 3-6 hours
3. Intermediate-Acting NPH (Humulin N and Novolin N) Onset: about 2 to 4 hours after injection
Peak: 4 to 12 hours later
Duration: it is effective for about 12 to 18 hours
4. Long-Acting insulin detemir (Levemir), insulin glargine
Onset: between 2 and 4 hours
Peak: long acting insulin has a continuous, “peakless” action that mimics the way your body normally releases insulin
Duration: last up to 24 hours
In 2015 an inhaled insulin product, Afrezza, became available in the U.S. Afrezza is a rapid-acting inhaled insulin. Afrezza must be used in combination with injectable long-acting insulin in patients with type 1 diabetes and in type 2 patients who use long-acting insulin.
5. Inhaled insulin Technosphere insulin-inhalation system (Afrezza) Onset: within 12 to 15 minutes
Peak: 30 minutes
Duration: Out of your system in 180 minutes
OTHER INJECTED MEDICATIONS
In addition to pills and insulin, some medications for controlling your blood glucose are injected.
1. Synthetic amylin pramlintide (Symlin)
Synthetic amylin slows food moving through the stomach. This can decrease appetite and may cause weight loss. It also reduces glucose
production by the liver. This keeps after-meal glucose levels from going too high.
2. GLP-1 analogues exenatide (Byetta and Bydureon), liraglutide (Victoza), albiglutide (Eperzan and Tanzeum), dulaglutide
(Trulicity)
GLP-1 analogues stimulate the release of insulin when blood glucose is high and decrease the amount of glucose produced by the liver.
They also slow food’s movement through the stomach, which decreases appetite and may lead to weight loss.
WHAT IF MY BLOOD GLUCOSE STAYS TOO HIGH?
If your blood glucose levels remain too high, your medication may need to be adjusted. Do not adjust your medication on your own. Talk to your doctor about possible changes.